Effect on diabetes standard of care 2 years after COVID pandemic
Internal Medicine Department, University of Jeddah, Saudi Arabia
*Corresponding Author:
Hani S. Shalabi,
Internal Medicine Department, University of Jeddah,
Saudi Arabia,
Email: hshalabi@uj.edu.sa
Received: 06-May-2023, Manuscript No. AJDM-23-97923 ;
Editor assigned: 08-May-2023, Pre QC No. AJDM-23-97923 (PQ);
Reviewed: 11-May-2023, QC No. AJDM-23-97923 ;
Revised: 11-May-2023, Manuscript No. AJDM-23-97923 (R);
Published:
15-May-2023, DOI: 10.54931/AJDM-31.3.1.
Abstract
Background: Diabetes mellitus (DM) is a chronic metabolic
disorder requiring long-term management to prevent complications.
The COVID-19 pandemic has impacted healthcare systems
globally, necessitating adaptations in care delivery. This
study explores the impact of the pandemic on DM care standards
from 2019 to 2022 by examining process and outcome
indicators.
Methods: A retrospective cohort study was conducted using a
quantitative approach, analyzing 12 indicators of DM care standards
among 9,423 adult patients diagnosed with type 1 or 2
diabetes mellitus attending an outpatient medical clinic.
Results: The results indicated consistently high scores for creatinine/
eGFR tests and low scores for referrals to clinic nutritionists.
The lipid profile check-up indicator displayed a declining
trend in measurements. Most indicators showed increased positive
scores in DM care standards after the COVID pandemic
(2022), with the exception of the lipid profile check-up.
Discussion: The findings suggest that while some aspects of
DM care have improved, other areas, such as nutritional counseling
and lipid profile check-ups, require further attention. Addressing
these gaps is crucial for ensuring comprehensive and
effective DM management, which involves raising awareness
among healthcare providers and providing necessary resources
and support.
Keywords
Diabetes Mellitus; COVID-19; Healthcare; Standards
of care; Chronic disease management
Introduction
Diabetes Mellitus (DM) is a chronic metabolic disorder
that affects millions of people globally. It necessitates
long-term management to avert complications such as
heart disease, kidney disease, and blindness.1 In various
settings, a combination of performance measures has been
linked to lasting improvements in certain aspects of diabetes care.2 However, the COVID-19 pandemic brought
about significant changes in healthcare systems, including
the implementation of telemedicine, a decrease in in-person
visits, and the reallocation of healthcare resources toward
COVID-19.3
This study seeks to explore the impact of the COVID-19
pandemic on DM care standards two years after its onset
by examining process and outcome indicators from 2019
to 2022. The research will utilize data from DM patients
referred to clinics for DM management. The data encompass
12 indicators of DM care standards, with the analysis
concentrating on the average percentage of each indicator
and any disparities between the years before, during, and
after the pandemic.
Materials and Methods
The investigation of the COVID-19 pandemic’s effects
on diabetes mellitus patients’ care standards was a retrospective
cohort study conducted using a quantitative
approach. 12 indicators were included: Dental referral,
ophthalmology referral, clinic nutritionist referral, urine
albumin checked, lipid profile checked, creatinine/eGFR
checked, HbA1c testing quarterly, HbA1c testing quarterly
checked for patients who attended the clinic quarterly,
urine albumin below target, HbA1c below target, LDL below
target, and creatinine/eGFR below target. The sample
comprised 9,423 adult patients diagnosed with type 1 or
2 diabetes mellitus who attended the outpatient medical
clinic from 2019 to 2022.
Results
Data was obtained from electronic medical records through
an integrated information system and then analyzed using
descriptive statistics in tables and graphs to compare the
results before, during, and after the COVID-19 pandemic.
Ethical approval was secured from the bioethics committee
for scientific and medical research at the University of
Jeddah (Table 1).
Table 1. Analysis and Results
| INDICATORS |
2019 (%) |
Average 2022 (%) |
Differences (%) |
| Dental Referral for Diabetes (%) |
9 |
11.00 |
2.00 |
| Urine Albumin checked (%) |
50 |
55.67 |
5.67 |
| Urine Albumin below target (%) |
36 |
42.67 |
6.67 |
| HBa1c below target (%) |
13 |
25 |
12.00 |
| Lipid profile checked (%) |
41 |
33.33 |
-7.67 |
| LDL below 100 mg/dl (%) |
59 |
60.00 |
1.00 |
| Ophthalmology (%) |
15 |
25.67 |
10.67 |
| HBa1c testing frequency tleast 4 times (%) |
5 |
12.33 |
7.33 |
| HBa1c testing frequency with 4 visit to the clinic (%) |
24 |
35.00 |
11.00 |
| Clinic nutritionist referral (%) |
3 |
7.67 |
4.67 |
| Creatinine eGFR checked (%) |
80 |
86.67 |
6.67 |
| Creatinine below target (%) |
21 |
33.67 |
12.67 |
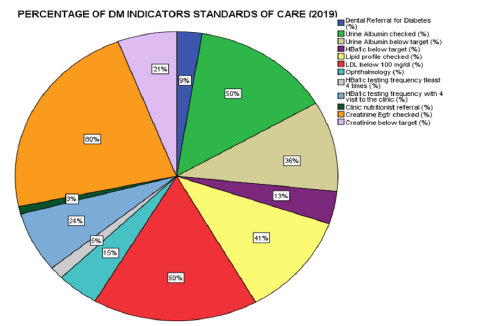
In the year prior to the pandemic (2019), the creatinine/
eGFR test had the highest percentage (80%), followed
closely by DM patients with their LDL below the target
(59%) (Figure 1). The lowest standards of care were observed
among DM patients referred to the clinic nutritionist
(3%) and those receiving HbA1c testing quarterly (5%).
Similar patterns were observed during the years of the
COVID pandemic (2020 and 2021) (Figures 2 and 3), with
the highest standards of care measurements from creatinine/
eGFR tests (82%) and DM patients with their LDL below 100 mg/dl (51% in 2020 and 53% in 2021). Lower
scores were also noted in referrals to the clinic nutritionist
(4%) and HbA1c testing quarterly (6%). These patterns
were also present before the COVID pandemic, showing
improvements in indicator measurements, except for
HbA1c below target (13% in 2019, 19% in 2020, and a slight
decrease to 15% in 2021). Additionally, there was no improvement
in the lipid profile indicator before and during
COVID, as it displayed a negative trend in measurements
(41% in 2019, 34% in 2020, and 29% in 2021). In 2022, the
quarterly indicator measurements revealed similar trends
(Figure 4), with the highest scores for creatinine/eGFR
checked (86.67%) and LDL below 100 mg/dl. The lowest
scores were observed in referrals to the clinic nutritionist
(7.667%) and dental (11%). When compared to the years
before COVID, there was an improvement in DM standards
of care measurements, with the highest improvement
seen in the HbA1c below target indicator, showing a
12% difference. The indicator with the least improvement
was the lipid profile checkup, which demonstrated a declining
trend from 2019 to 2022.
The observed trends in DM standards of care indicators
showed that the creatinine/eGFR check-up indicator consistently
had the highest scores from 2019 to 2022, while
the lowest scores were recorded for referrals to the clinic
nutritionist. The only indicator that showed a decrease in
scores after COVID (2022) was the lipid profile check-up,
which exhibited a declining trend in measurements over
the years. In contrast, all other indicators displayed increased
positive scores in the standard of care among DM
patients after COVID (2022).
Discussion
The analysis of the results reveals several interesting
trends regarding the standard of care among DM patients.
The consistently high scores for creatinine/eGFR tests
across the years indicate that this aspect of DM care has
remained a priority and is being adequately addressed.
However, the consistently low scores for referrals to the
clinic nutritionist and the declining trend in lipid profile checkups suggest that there are still areas within DM care
that need further improvement and attention.
It is worth noting that the COVID pandemic had an impact
on various aspects of DM care,4 as seen through the
fluctuations in the indicator measurements. Despite the
challenges posed by the pandemic, the standard of care
among DM patients generally improved in several aspects,
as evident by the increased positive scores in most of the
indicators after 2022. This improvement could be attributed
to the increased awareness and importance placed on
managing chronic conditions like diabetes during the pandemic.
The improvement in the HbA1c below target indicator is
particularly significant, as it demonstrates better glycemic
control among DM patients. This is an essential aspect of
diabetes management, as good glycemic control can significantly
reduce the risk of diabetes-related complications.
The consistently low scores in referrals to the clinic nutritionist
highlight the need for better integration of nutritional
counseling and support in DM care. Nutrition plays
a critical role in diabetes management, and these results
suggest that this aspect of care may not be receiving the
attention it deserves. Addressing this gap could lead to
better overall outcomes for DM patients, as proper nutrition
guidance can help patients make healthier choices
and manage their condition more effectively.
The declining trend in lipid profile checkups is another
area of concern, as regular monitoring of lipid levels is
essential for DM patients to manage their cardiovascular
risk. The decrease in scores may indicate that there is a
need for better awareness among healthcare providers
and patients about the importance of regular lipid monitoring
in diabetes care.
Interestingly, the results show improvements in most of
the indicators after the COVID pandemic, despite the challenges
it brought to healthcare systems globally. This may
indicate that healthcare providers and patients adapted to
the new circumstances, and, in some cases, even enhanced
their focus on managing DM. However, further research
is needed to explore the specific factors that contributed to
these improvements.
The study’s limitations include its retrospective nature,
which depends on pre-existing data and may lead to biases
or discrepancies in the results. Additionally, the research
is based on data from a single outpatient medical clinic,
which restricts the applicability of the findings to other
contexts. The quantitative methodology employed in the
study might not capture the subtleties of patient experiences
or healthcare provider perspectives, as it does not
include qualitative data. Moreover, potential confounding
variables such as changes in healthcare policies, resource
availability, and patient adherence to treatment guidelines
were not taken into account, which could have impacted
the observed trends. Although the study provides valuable
insights into the effects of the COVID-19 pandemic on
DM care standards, these limitations should be considered
when interpreting the results. Future research addressing
these limitations may contribute to a more thorough understanding
of the pandemic’s impact on DM care,5 and inform strategies for enhancing patient outcomes.
Conclusion
This study provides valuable insights into the impact of
the COVID-19 pandemic on diabetes mellitus care standards
from 2019 to 2022. The results indicate that, despite
the challenges posed by the pandemic, several aspects of
DM care have improved, such as glycemic control. However,
areas such as nutritional counseling and lipid profile
check-ups still require attention and improvement to ensure
comprehensive and effective diabetes management.
The study highlights the need for ongoing vigilance in addressing
gaps in DM care and raising awareness among
healthcare providers and patients about the importance
of a holistic approach to managing this chronic condition.
Moreover, it emphasizes the importance of providing necessary
resources and support to maintain and improve
DM care standards, even in the face of global health crises.
Future research should focus on addressing the limitations
of this study and exploring the specific factors
contributing to improvements in DM care standards after
the COVID-19 pandemic, ultimately guiding strategies to
optimize patient outcomes in the long term.
References
- World Health Organization. Global Report on Diabetes. Geneva: WHO; 2016
- O'Connor PJ, Bodkin NL, Fradkin J, et al. Diabetes performance measures: Current status and future directions. Diabetes Care; 2011:34:7:1651-9
[Crossref] [Google Scholar] [Pubmed]
- Wang X, Zhang X, Tang Y, et al. The prolonged COVID-19 pandemic caused significant psychosomatic symptoms in frontline healthcare workers. Psychiatry Res; 2023:321:115060
[Crossref] [Google Scholar] [Pubmed]
- Stone BM. The explanatory ability of COVID-19 life changes on quality of life: A comparison of those who have had and not had COVID-19. Curr Psychol; 2022:4:1-12
[Crossref] [Google Scholar] [Pubmed]
- Coombs C. Autistic study consultants can help when results don't replicate. Spectrum; 2021