Paediatric endocrinology and diabetes mapping and services in Nigeria: A decade after
*Corresponding Author:
Received: 31-Jan-2022, Manuscript No. ajdm-22- 55667;; Accepted Date: Feb 25, 2022 ; Editor assigned: 02-Feb-2022, Pre QC No. ajdm-22- 55667 (PQ); Reviewed: 16-Feb-2022, QC No. ajdm-22- 55667;; Revised: 21-Feb-2022, Manuscript No. ajdm-22- 55667 (R); Published: 28-Feb-2022, DOI: 10.54931/2053-4787.30-2-1
Abstract
Purpose: Paediatric endocrinology services are relatively new in Africa and Nigeria and the services and resources for the children with diabetes and other endocrine disorders are poorly developed. We aimed to survey pediatric endocrinology services in Nigeria using an online survey tool.
Methods: We surveyed the paediatric endocrinologists practicing in public tertiary institutions in Nigeria using an instrument designed to evaluate the availability of manpower, infrastructures, specific medications, and collaborations with other endocrinologists.
Results: Fifteen of the 37 practicing paediatric endocrinologists responded, giving a response rate of h a response rate of 40.5%. The mean practice years was 9.3 (range 7-12), and many had skills in managing children with diabetes, thyroid and growth abnormalities. All centres had facilities for ultrasound scan and simple diagnostic techniques but few centres had access to iodine uptake studies, antibody testing and special hormones. While most centres could outsource special tests, patients could rarely afford the services. There were 297 children on management for TIDM and over 90% of these were on pre-mix insulin.
Conclusion: The dearth in human and infrastructural capacity in paediatric endocrinology services should be improved on and this will alleviate the burden of diabetes and endocrine disorders in Nigerian children.
Keywords
Paediatric endocrinology, Diabetes, Services, Nigeria
Introduction
Diabetes and other endocrine disorders are gradually increasing in prevalence in Africa and Nigeria and it only means that the services and infrastructures to help manage these cases should grow and improve to meet the demands of the children.1-4 In Sudan, the estimated incidence of diabetes mellitus in children is 10.1/100,000 which is possibly the highest in Africa.5,6 Paediatric endocrinology services in Nigeria started over 24 years ago when the first fellow graduated from training in Canada. This fellow served as the only Paediatric endocrinologist in Nigeria for well over 15 years until the European Society for Paediatric Endocrinology (ESPE), the International Diabetes Federation (IDF) and International Society for Paediatric and Adolescent Diabetes (ISPAD) started a training school in Africa for Paediatric endocrinology in 2008.7-9 Subsequently, another training school started in Nigeria for the West African sub region in 2012. Since their inception, over 35 fellows have been trained in Nigeria alone with more than 85 fellows in Africa, several of who have worked tirelessly to meet the endocrine and diabetes needs of children while also conducting researches in the field.8,10-13
Nigeria’s population is well over 211 million and 43.3% of these are children less than 15 years old 6,14 and 51% of these children live in the urban areas leaving 40% in the rural areas with poor access to health care and other basic facilities. There are no incidence rates of childhood diabetes but anecdotal studies estimate 1, 500 children being cared for with diabetes. There is lack of data for other endocrine disorders as well, however, short stature is quite prevalent in the Nigeria, with an estimated 37% children population being stunted and how many of these are due to endocrine disorders is unknown.13,15 The population growth rate is high but the physician numbers are low in comparison and most of the brighter ones are immigrating to other countries, thereby worsening the health care need in the nation. The insecurity in the Northern part of Nigeria also contributes to the reduced medical workforce for the population already grappling with dearth in resources and infrastructure thereby worsening health care delivery and health indices.13,16,17
The Paediatric endocrinology training in Africa and West Africa by the European tutors were mostly clinical, with ward rounds of admitted patients, clinic consultations, stimulation tests, and didactic lectures, seminars, workshops and journal reviews.17,18 They followed the syllabus and curriculum of the European Society for Paediatric endocrinology. Examinations and thesis defense were conducted for each fellow to evaluate the competence and proficiencies of these fellows. These trainings were supplemented with trainings in more specialized centers in Europe for about 3 to 6 months for most fellows who got scholarships to attend these clinical fellowships. The fellows were expected to return to their home institution to start up endocrine services or standardize service delivery where they already exist. In resource limited settings, delivering Paediatric endocrine services can be a challenge due to an existing background of limited laboratory support, medications and availability of equipment. The aim of this survey is to evaluate Paediatric endocrinology care in Nigeria in terms of availability of facilities and resources. The result of this survey will be used in seeking and improving Paediatric Endocrinology care in various regions in Nigeria.
Methods
This study was a cross sectional survey involving all Paediatric endocrinologist who were in the Society for Paediatric and adolescent endocrinology in Nigeria (SPAEN) data base. As at the time of the survey, there were 37 practicing paediatric endocrinologists in Nigeria, and 15 responded to the survey questionnaire. Giving a response rate of 40.5% the instrument was pretested with 3 paediatric endocrinologists who are not part of the final respondents. There were 6 parts of the questionnaire, demographics and hospital settings, infrastructure availability, drugs/medication availability, clinic strengths of specific conditions including diabetes mellitus, collaborations with other institutions in Nigeria and abroad. Also retrieved were the challenges individual respondents faced in managing their patients in the clinics.
Completed surveys were analysed and multiple responses from the same institutions were reviewed with follow up telephone interviews to clarify information. Ethical approval for exemption was obtained from the Research and Ethics committee of the University of Port Harcourt Teaching Hospital. Information or responses were entered into excel sheet and analysed using SPSS version 23.
Result
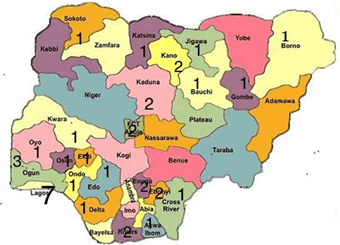
Fifteen paediatric endocrinologists responded to and completely filled the questionnaire representing the 6 geopolitical areas of Nigeria, though there are 37 paediatric endocrinologists in Nigeria (Figure 1). The years of practice ranged from 8-12 years and about half of these respondents had some clinical fellowship experience in European hospitals (Table 1). Many respondents indicated proficiency in managing diabetes mellitus; short stature, thyroid disorders, bone and pubertal disorders and 40% agreed they had difficulties in making pathological diagnosis of children with disorders of sex developments.
Figure 1. Map of Nigeria with trained and board-certified paediatric endocrinology fellows. There are 37 endocrinologists but they are not evenly spread across the country with most in the South West region. While this number indicates a net increase of 97.3% from 1992 till date, there are only 13 paediatric endocrinologists in Northern Nigeria and 24 in Southern Nigeria.
| Unit | Practice years | Expertise | PETCA | EUR FELLOW | MENTOR | INT’MEM | INT RES |
|---|---|---|---|---|---|---|---|
| PHC | 12 | THY, DSD, DM | YES | YES | ISRAEL | YES | YES |
| KANO | 8 | DM, THY, BONE | PWA | NO | NO | NO | NO |
| GOMBE | 9 | DM | YES | YES | AUSTRA | NO | YES |
| SOKOTO | 8 | DM | PWA | NO | NO | NO | NO |
| BENIN | 8 | DSD, THY, DM | PWA | NO | GERMANY | YES | YES |
| ZARIA | 11 | DSD, BONE, GROWTH | YES | YES | ISRAEL | YES | YES |
| IFE | 12 | DSD, DM, THY | YES | YES | ISREAL, POL | YES | YES |
| ABUJA | 8 | DM, THY | PWA | NO | NO | NO | YES |
| PETCA: Paediatric endocrinology training in Africa, PETCWA: Paediatric endocrinology training center for West Africa, EUR FELLOW: Attended 3 – 6 months Clinical fellowship in Europe, INT MEM member of International Paed Endo society, INT RES: International research participant. | |||||||
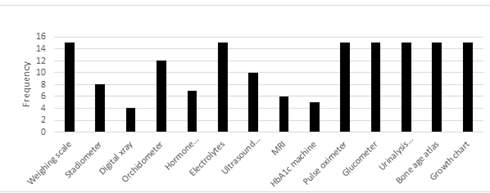
Standard equipment for endocrinology
Eight of the 15 respondents had standardized stadiometer in their clinics, with the remaining having to use improvised tape measures for height measurement. All centers had growth charts, glucometers, urine ketone strips and atlas for bone age. While all centers have regular X-ray machines, only 4 have digital X-ray machine.
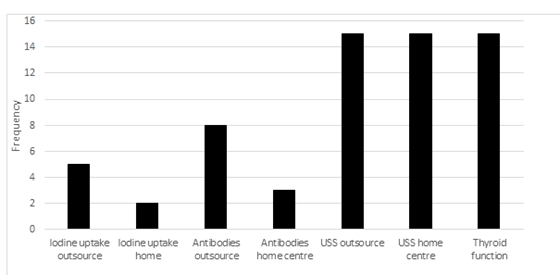
Thyroid
Assessing the availability of instruments for evaluating thyroid disorders and the competence of respondents, the survey revealed that all centers could do basic thyroid function tests TSH, fT4 and fT3, but had to outsource antibody testing using peripheral laboratories that were expensive and out of reach to most of the patients. There were radiologists who could do ultrasound scan of the thyroid gland though, 60% of the respondents needed to have second opinion of the radiologists’ reviews. Only 2 of the respondents could do thyroid ultrasound scans themselves but all believed having the skill, and proficiency is essential for services and training. One respondent had a point of care ultrasound scan machine in his clinic, and one center had the ability to do iodine uptake studies.
Diabetes mellitus clinic strengths
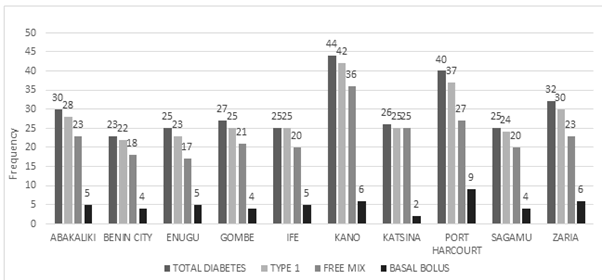
All clinics have patients with diabetes, thyroid disorders, pubertal abnormalities and short stature. In the 10 centres surveyed, there were a total of 297 children with diabetes and 94.6% are type 1 Diabetes mellitus patients. Many patients use free-mix insulin, 230 (77.4%) while only few, 50 (16.8%) use basal bolus regimen. Zaria and Kano have the largest number of patients using basal bolus regimen.
Discussion
The number of paediatric endocrinologists
There are 37 trained and board certified paediatric endocrinologists in Nigeria, many of whom were trained in the last 9 years under European and American tutors. This is a great feat coming from an era of just one paediatric endocrinologist before the turn of the last decade to 37, with sponsorships from the International Diabetes federation, European Society for Paediatric endocrinology and International Society for Paediatric and Adolescent Diabetes. However, taking this information in another perspective of need, the number is grossly inadequate for the many children in Nigeria needing endocrine services and is not entirely different from what is obtainable is other disciplines.
There is a concentration of the endocrinology fellows in the South (SW, SE, and SS) but only pockets in the North, with little or no presence in the North Central. The population of children in Northern Nigeria is higher than that in the South and with the recent terrorism and insurgency, many of these Northern children with needs for growth evaluation and treatment of other endocrine disorders will go without these services.13,16,17 The population of board certified and clinically active paediatric endocrinologist in North America in 2011 was 886 for a population of 73 million giving a ratio of 21 clinically active paediatric endocrinologists per 1 million children.10,19 The population of children in Nigeria in 2017 as projected was 87 million giving a ratio of 1 board certified paediatric endocrinologists for every 1,650,000 children. For equity, there has to be a method of continuous training of paediatric endocrinologists to provide and indeed, improve the service delivery in Nigeria and most likely other parts of Africa as suggested by Rowland et al.20,21
Developing centers of excellence in parts of Nigeria will increase the number of training centers so more fellows of the Post graduate medical Colleges of Nigeria and West Africa will undergo tutelage for a minimum period of 1 year and get certified. For this to happen, the minimum standards must be attained and maintained. There is no doubt that Lagos and Nairobi are standards now, and continuous training will possibly improve these with minimal donor sponsorship. For this to happen though, there must be availability of support equipment and staff including Glucometers, HbA1c machines, urinalysis, stadiometer etc., for standard clinic functioning.
Equipment for service delivery and training
All centers have basic equipment for the provision of services and training like glucometers, urinalysis, bone age atlas, weighing scale but few had standard stadiometers as recommended by the ESPE curriculum.17,18. Laboratory services are also available for electrolytes including calcium, phosphate and alkaline phosphatase, but the results of these are not retrieved as fast as they are needed. While some centers can get their results within hours, many have to wait for 24-48 hours, thereby limiting the judgment or management protocols that can be instituted for the patients. No center does blood gas analyses, iodine uptake studies, or antibody testing but many can outsource these from peripheral laboratories in and around their home states. The costs of these are however prohibitive and are not affordable to many of the patients making it pertinent that Government should provide these services in the tertiary hospitals at subsidized rates. In a country where only 4% of its population have health insurance with standard coverage, and most patients pay out of pocket, getting to do these tests will be not be feasible and it is little wonder many of the patients are lost to follow up.17 Radiology is an important adjunct discipline in the practice and management of endocrine disorders. Manual X ray machines are still being used in many centers but four centers have digital radiograph machines with which digital images can be sent to physicians computers and other specialized softwares can be used to read the films. All respondents sought second opinions with regards to radiologist’s consults because the information provided were likely incongruous with the clinical features. The most common inconsistency is the bone age reports from radiologists which either under or over-estimated the bone ages of patients. Participants use either the Guerlisch and Pyle or Tanner Whitehouse methods to estimate bone ages of patients.21-25
All centers have ultrasound scan machines, with skilled radiologists to manage this service but only one has point of care USS. USS helps to check the structural integrity or abnormalities of endocrine organs and tissues and with newer techniques, functionality may be inferred from what is seen on the screens. While all of the respondents agreed that USS machines should be available in all clinics and all endocrinologists should be competent in using these machines, only two have been trained and certified on thyroid and other endocrine system scanning. In house MRI machine was available in only 4 centers and can be outsourced for many of the other centers, though cost becomes an issue. It must be mentioned at this point that the non-availability of these equipment did not prevent the clinical diagnoses of many diseases, but optimal and standardized management may not have been met in most diseases. All clinics had orchidometers for estimation of testicular sizes and puberty evaluation, and this is mostly courtesy of their training in PETCWA and PETCA. This again makes the discussion of having many centers accredited for training pertinent as smaller and less expensive instruments can be purchased or sourced for. While increasing service delivery, training facilities will be improved for stimulation tests, diagnostics and treatment.
Diabetes mellitus diagnosis has increased in Nigeria steadily mostly because of the increased number of specialists and awareness and also because of the improved diagnostic processes. There is no national prevalence yet but individual centres have reported increased hospital consultations and admissions for DKA. No center in Nigeria is using the insulin pump and that can be understood from the perspective of suitability, affordability and maintenance of the machine.20,21 Many however use the free mix insulin for management of diabetes mellitus though there is the transition of patients to the basal bolus regimen using long acting and rapid acting insulin and the uptake by patients is relatively encouraging (Figure 2). In resource replete settings where insulin pumps are being used, the insurance services pay for them and from the survey here in Nigeria, all children with endocrine conditions have their parents paying out of pocket for services and devices for blood glucose testing and insulin.17
Figure 2. Frequency distribution of diabetes mellitus cases and types of insulin regimen used in some paediatric endocrine units in Nigeria. Kano state had the highest number of diabetic patients, 44 followed by Port Harcourt, 40 with the least being Benin-City, 23. Basal bolus was used mostly by children from Zaria, 19 followed by those in Port Harcourt, 9. A large number of children still use pre-mix insulin in all centers managing diabetes mellitus.
Clinic strengths
The first school of paediatric endocrinology started 9 years ago in Nairobi and has evaluated 1,399 children for various endocrine disorders as of 2015.7,8 The first year of commencement had only 108 children and this number gradually increased till the present Figure 3. In Nigeria, most paediatricians practice general paediatrics and combine this with endocrinology and other sub specialties and this is understandable because there is still a dearth of board certified paediatricians. The numbers may seem small at this time but we must bear in mind that these clinics are relatively new, with few referrals and only the Western centers like Lagos, Ibadan and Ile-Ife have outposts (community) for paediatric endocrinology. This community endocrinology must be encouraged to increase the yield and service delivery to those who have difficulty getting to the tertiary centers.7-9 PETCA in Nairobi and Botswana fellows also have outposts that serve the less privileged to some extents.
Improving yield and capacity building
This survey has shown that there is need for more paediatric endocrinologists in Nigeria which must be filled in the next few years to close the gap between demand and supply. With greater awareness of the general population of endocrine disorders and diabetes, many referrals will be made and the few endocrinologists will become overwhelmed. The good news is that most of these are younger fellows who have many years to practice clinical medicine. On the flip side is the exodus of general paediatricians and fellows in training to more comfortable and user friendly environments leaving fewer paediatricians for a growing population.6,22,26-28 Setting up standard endocrinology clinics that can train up to 2 fellows in a period of 15 months as done in PETCA and PETCWA will increase this number greatly and this should be the goal of post graduate colleges and boards. So, if 10 centres are made to provide this training, we are likely to have over 50 board certified endocrinologists in 5 years.
Starting weekly or twice monthly community outpost clinics can also improve the impact felt by the society and educating these people will make for better understanding of the diseases and their presentations. Lagos and Oyo states have community outpost centers that have been running for over 4 years now and this has increased the number of patients being seen in these centers. The continuous visits of physicians to these centers will also remove myths and legends that mar the proper management of these conditions and thereby reduce mortality. With community services, children with other conditions that are not endocrine can be evaluated and referred appropriately to their various subspecialties. Endocrinologists should also be alert to changing disease patterns in communities that can be communicated to authorities for research and proper recommendations made.
The most important yet challenging proactive intervention to improving the yield is purchase of equipment and basic instrument for care of children with endocrine disorders (Figure 4). It is well known in the medical community that endocrine diseases are one of the most expensive and long term diseases. It is at this point that Government and donor agencies must come together to do a needs assessment and work out modalities for equipment leasing, private public partnership, or outright donation with memoranda of understanding for maintenance and sustainability.
Board review courses and recertification
Like many other disciplines in medicine and paediatrics, board review courses should be incorporated into yearly practice licensing of all paediatric endocrinologists in Nigeria and the original training institutions or fellowship providers should supervise this.10,17-19 This way, confidence is built over time within and outside the training institutions and referrals can go back and forth like is already being done with mentees and mentors among the trainers. ESPE provides educational materials on its website including case scenarios with questions and answer sessions and vignettes that are home grown with suggestions on management options available based on the resources available. Now, knowing that endocrine disorders are expensive to investigate and diagnose, cost effective measures are suggested for the physician for many endocrine conditions and these vignettes are available for free.
Recently, a summer school programme has been introduced to the yearly African society for Paediatric and Adolescent endocrinology meetings and in this programme, attendees are made to provide case reports of endocrine conditions and discussions around these cases are done with faculties from ESPE, ISPAD and PES. Faculties make suggestions on how to do more with less and still achieve standard or near standard management goals. This is another way of providing continued medical education and review certification to fellows practicing in resource limited settings, like Nigeria.
Conclusion
While so much has been achieved in improving the services for paediatric endocrinology in Nigeria, it is like a flash in the pan considering the population of children that need to be covered. Training more paediatric endocrinologists and recertification will need to be scaled up within the next decade for equity to be achieved. Improving the equipment already available and providing more for basic clinical, and pathologic diagnoses of conditions can be achieved in the tertiary training health care institutions.
Key Objective
Diabetes and other endocrine disorders in Nigeria are increasing gin prevalence with the attendant need for human and capital resources to help manage these children. The study aimed to evaluate what human, and/or capital resources and services are available in Nigeria.
Though there are few board certified paediatric endocrinologists, the inequitable distribution with more of them in the southern part of Nigeria and the poor infrastructural development may worsen the plight of the Nigerian child.
Relevance
The study may help stakeholders and health policy makers in Nigeria improve the training of paediatric endocrinologists and also redistribute them to areas of dire need.
Acknowledgment
Authors acknowledge the paediatric endocrinologists that took time out to complete the survey despite their busy schedules.
Conflict of Interest
The authors declare no conflicts of interest with this research.
References
- Elamin A, Ghalib M, Eltayeb B. High incidence of Type I diabetes mellitus in Sudanese children, 1991-1995. Ann Saudi Med. 1997;17(4):478-80.
- Motala AA, Omar MAK, Pirie FJ. Epidemiology of type 1 and type 2 diabetes in Africa. Euro J Prev Cardio. 2003;10:77-83.
- Jaja T, Yarhere I. The pattern of presentation and trends of childhood diabetes mellitus in Port Harcourt, Southern Nigeria. J Adv Med Med Res. 2015;5(2):247-253.
- Hawley NL, Rousham EK, Norris SA. Secular trends in skeletal maturity in South Africa: 1962–2001. Ann Hum Biol. 2009;36(5):584-594.
- Saad FM, Mahmoud LA, Ali AMM. Incidence and prevalence of type 1 diabetes mellitus in children and adolescents aged 6 months–19 years in Khartoum State, Sudan. Sudanese J Paediatr. 2020;20(20):163-169.
[Cross Ref] [Google Scholar] [PubMed]
- Ahmed H, Elshaikh T, Abdullah M. Early diabetic nephropathy and retinopathy in patients with type 1 diabetes mellitus attending Sudan childhood diabetes centre. J Diabetes Res. 2020;24.
[Cross Ref] [Google Scholar] [PubMed] [Research Gate]
- Odundo GO, Ngwiri T, Otuoma OLP. the impact and successes of a paediatric endocrinology fellowship program in Africa. Intl J Endocrinol. 2016.
[Cross Ref] [Google Scholar] [Pub Med]
- Beshyah SA KAB, Sherif IH, Benbarka MM, et al. A survey of clinical practice patterns in management of Graves disease in the Middle East and North Africa. Endocr Pract. 2016;23:299-308.
[Cross Ref] [Google Scholar] [PubMed]
- Odundo GO, Ngwiri T, Otuoma OCNM. Developing equity in capacity of paediatric endocrinology subspecialists worldwide. Lancet Diabetes Endocrinol. 2016; 4: 204-205.
- Jaja T, Yarhere IE. Clinical characteristics of children and adolescents with thyroid disorders seen at the University of Port Harcourt Teaching Hospital: A five year review. Nig J Paediatr. 2014;41:302-306.
- Yarhere IE, Jaja T, Oduwole A, et al. Normative thyroid-stimulating hormone values for healthy Nigerian newborns. Horm Res Paediatr. 2016; 85:22-28.
[Cross Ref] [Google Scholar] [PubMed]
- Yarhere IEJT, Briggs DIL. Newborn screening in Nigeria: will incorporating congenital hypothyroidism with sickle cell disease improve neonatal screening programme. Acta Bio Medica. 2019;90:316-320.
[CrossRef] [Google Scholar] [PubMed]
- Chukwuma A, Ehator-Mobayode UE. Armed Conflict and Maternal Health Care Utilization. Soc Sci Med. 2019;226:104-112.
[CrossRef] [Google Scholar] [PubMed]
- United Nations (2021) World population dashboard Nigeria.
- National Population Commission NPC and ICF. Nigeria Demographic and Health Survey 2018 Key Indicators Report. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF. 2019.
- Olarewaju OA. Insecurity in northern Nigeria: Implications for maternal and child health. Clinical Epidemiology and Global Health. 2021;12.
- Alawode GO, Adewole DA. Assessment of the design and implementation challenges of the National Health Insurance Scheme in Nigeria: a qualitative study among sub-national level actors, healthcare and insurance providers. BMC Public Health. 2021;124:1-12.
[Cross Ref] [Google Scholar] [PubMed]
- Busiaha KPA, Tornesec G, Weintrobd N, et al. European Training Requirements for Competency in Paediatric Endocrinology and Diabetes 2021. Horm Res Paediatr. 2021;94:441-447.
[Cross Ref] [Google Scholar] [PubMed]
- Vigersky RA, Fish L, Hogan P, et al. The Clinical Endocrinology Workforce: Current Status and Future Projections of Supply and Demand. JCEM. 2014;99:3112-3121.
[Cross Ref] [Google Scholar] [PubMed]
- Rowlands A AE, Rutagarama F, Dipesalema J, et al. Insights from the WHO and National Lists of essential medicines: Focus on pediatric diabetes Care in Africa. Horm Res Paediatr. 2018;90:82-92.
[Cross Ref] [Google Scholar] [PubMed]
- Adeniyi MA, Efuntoye O, Popoola G, et al. Profile and determinants of intention to migrate by early career doctors in Nigeria: A report from CHARTING study. Int J Health Plann Manage. 2022.
[Cross Ref] [Google Scholar] [PubMed]
- Gertych A ZA, Sayre J, Pospiech-Kurkowska S. Bone age assessment of children using a digital hand atlas. Comput Med Imaging Graph. 2007; 31:322-331.
[Cross Ref] [Google Scholar] [PubMed]
- Martin DD, Witt JM, Hochberg Z. The use of bone age in clinical practice–part 1. Hormone research Pediatr. 2011;769(1):1-9.
[Cross Ref] [Google Scholar] [PubMed]
- Abdullah MA, Saeed U, Abass A, et al. Disorders of sex development among Sudanese children: 5-year experience of a pediatric endocrinology clinic. J Pediatr Endocrinol Metab. 2012;25:1065-1072.
[Cross Ref] [Google Scholar] [PubMed]
- Govender D, Goodier M. Bone of contention: The applicability of the Greulich–Pyle method for skeletal age assessment in South Africa. South Afr J Radiology. 2018.
[Cross Ref] [Google Scholar] [PubMed]
- Hallock JA, Mckinley DW, Boulet JR. Migration of doctors for undergraduate medical education. Med Teach. 2007;29:98-105.
[Cross Ref] [Google Scholar] [PubMed]
- Healy GO. A global link between national diversity policies? The case of the migration of Nigerian physicians to the UK and USA. Int J Human Resource Manag. 2007;18:1917-1933.
- Awire E, Okumagba MT. Medical education in Nigeria and migration: a mixed-methods study of how the perception of quality influences migration decision making. Med Ed Publish. 2020;9:1-13.