Thiazolidinediones: Understanding Their Role in Diabetes Management
*Corresponding Author:
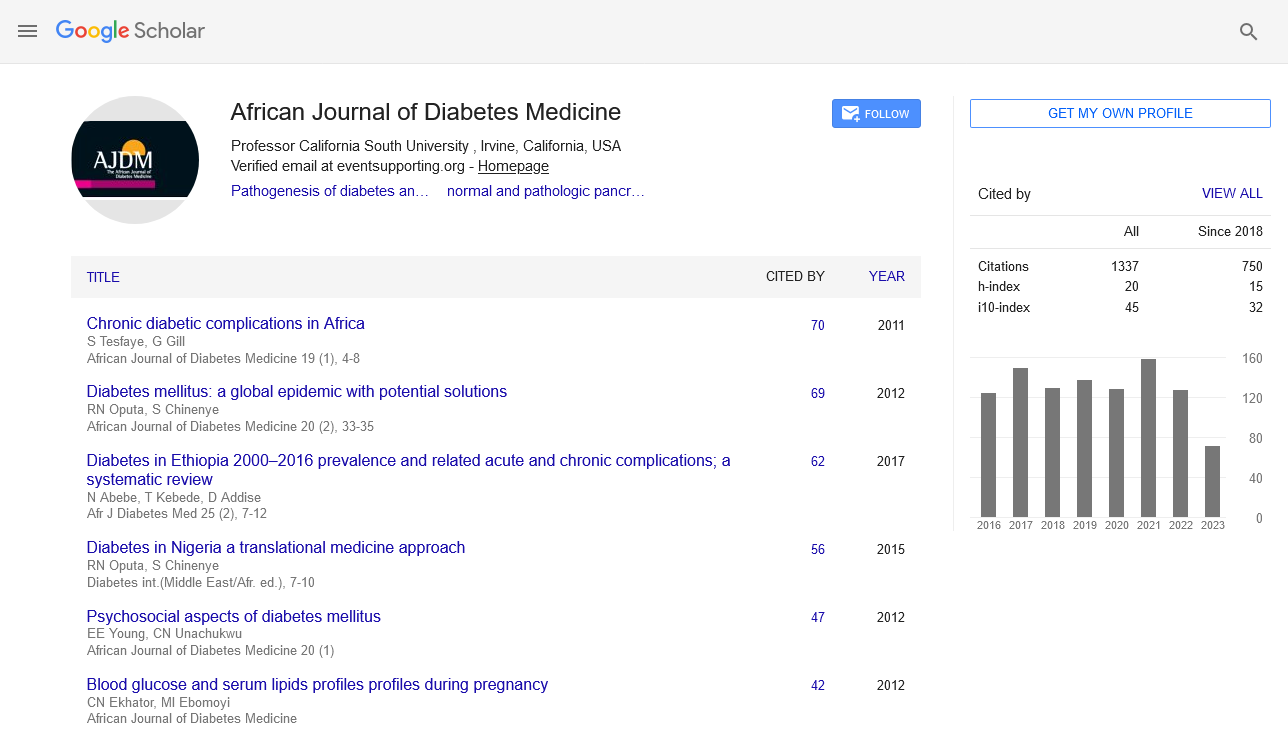
Received: 29-May-2024, Manuscript No. ajdm-24-143108; Editor assigned: 31-May-2024, Pre QC No. ajdm-24-143108 (PQ); Reviewed: 14-Jun-2024, QC No. ajdm-24-143108; Revised: 19-Jun-2024, Manuscript No. ajdm-24-143108 (R); Published: 26-Jun-2024, DOI: 10.54931/AJDM-32.3.4.
Introduction
Thiazolidinediones (TZDs), also known as glitazones, constitute a class of medications used primarily in the treatment of type 2 diabetes mellitus. These drugs work by targeting insulin resistance, a key feature of type 2 diabetes where the body’s cells become less responsive to insulin. By enhancing insulin sensitivity in peripheral tissues, TZDs help improve glucose uptake and utilization, thereby aiding in the control of blood sugar levels. This article explores the mechanisms of action, clinical applications, potential benefits, and considerations associated with thiazolidinediones in diabetes management.
Description
The primary mechanism through which thiazolidinediones exert their therapeutic effects involves activation of peroxisome proliferator-activated receptor gamma (PPARγ), a nuclear receptor found in adipose tissue, skeletal muscle, and liver cells. Activation of PPARγ results in several beneficial effects. PPARγ activation leads to increased expression of genes involved in glucose uptake and utilization in muscle cells, as well as decreased hepatic glucose production. This helps lower blood glucose levels by improving insulin sensitivity at the cellular level. Thiazolidinediones can also improve lipid profiles by reducing triglycerides and increasing highdensity lipoprotein (HDL) cholesterol levels. This dual effect on both glucose and lipid metabolism contributes to their role in managing cardiovascular risk factors associated with diabetes. Thiazolidinediones are typically prescribed as adjunctive therapy to other antidiabetic medications, such as metformin or sulfonylureas, when these agents alone are insufficient to achieve adequate glycemic control. They are particularly beneficial in individuals with type 2 diabetes who exhibit significant insulin resistance and may not respond well to insulin-sensitizing lifestyle modifications alone. TZDs are effective in lowering HbA1c levels, a marker of long-term glucose control, by addressing insulin resistance directly. There is evidence suggesting that TZDs may help preserve pancreatic beta-cell function, which is responsible for producing insulin. This preservation is crucial in delaying the progression of diabetes and reducing the need for exogenous insulin therapy. Beyond their glycemic benefits, thiazolidinediones have been associated with improvements in endothelial function, reduction in inflammatory markers, and potential cardiovascular risk reduction. These effects make them valuable in managing diabetes-related complications, such as coronary artery disease and stroke. While generally well-tolerated, thiazolidinediones are not without potential side effects and considerations. One of the most common side effects of TZDs is fluid retention, which can lead to edema (swelling). This side effect is more pronounced with certain members of the class, such as rosiglitazone. Thiazolidinediones can cause mild to moderate weight gain due to fluid retention and increased adipogenesis (formation of fat cells). This effect should be monitored, especially in patients prone to cardiovascular complications. Long-term use of TZDs has been associated with a small increase in the risk of fractures, particularly in postmenopausal women. Regular assessment of bone density and consideration of alternative treatments may be necessary in individuals at high risk of osteoporosis. Periodic monitoring of liver enzymes is recommended during TZD therapy, as rare cases of liver toxicity have been reported. The role of thiazolidinediones in diabetes management continues to evolve with ongoing research and clinical trials. Future directions include exploring their potential in combination therapies, personalized medicine approaches based on genetic profiles, and understanding their effects on various metabolic pathways beyond glycemic control.
Conclusion
In conclusion, thiazolidinediones represent an important therapeutic option in the treatment of type 2 diabetes mellitus, offering significant benefits in improving insulin sensitivity, glycemic control, and potentially reducing cardiovascular risks. Their mechanism of action through PPARγ activation underscores their unique role in addressing insulin resistance, thereby complementing existing treatments and enhancing overall diabetes management strategies. As with any medication, the decision to prescribe thiazolidinediones should be individualized, taking into account the patient’s specific clinical profile, potential risks, and benefits in achieving optimal outcomes in diabetes care.